In 1950, Belgian men could not expect to become older than 65 years. A boy born in 2018, however, was expected to reach almost 80. In the same period, global life expectancy increased from 48 years to 67 years. The development of the polio vaccination in 1953 by J. Salk, for example, influenced life expectancy, as it prevented millions of premature deaths. Advancing medical technology has always relied on an evidence based approach. Today, we see the dawn of a new step in this evolution. Since data and the processing thereof has become exponentially more available, promising new opportunities are becoming attainable.

Challenges and opportunities
In 2013, Hollywood actress Angelina Jolie underwent a double mastectomy, even though there were no signs of breast cancer. Jolie had here DNA sequenced and discovered she carries a mutation of the BRCA1 gene that is associated with increased breast cancer occurrence. She decided on the surgical procedure was to prevent possible future illness.
This case is a telling example of two trends in the practice of advancing medical technology: medicine becomes personalized and preventive medicine gains importance. Traditionally procedures and dosages are tested and optimized for the average patient, however, it is now possible to tailor these procedures and dosages to the individual patient. The dramatic reduction in the cost of sensors, data communication and storage allows for meticulous tracing of the patients’ health, so illnesses can even be detected before they notice any symptoms. This preventive treatment of ailments can reduce costs considerably, both financially and in human suffering.
The spectacular increase in life expectancy brings challenges, as well. In 2050, one third of Belgians will be older than 60 years. Similar predictions are made for other European countries, which will put pressure on government health services and health insurance companies. Challenges of health services and insurance companies will need medical innovation to optimize treatment efficiency and quality.
AI and data science
What is AI, and what is it not
Artificial Intelligence (AI) covers a wide range of techniques that use the increasing computational power and reduced cost of data acquisition and storage. These techniques perform tasks that traditionally required human intelligence, such as interpretation of image and sound, taking decisions based on data, recognizing patterns, classification, searching and optimizing.
What can AI do?
Artificial Intelligence can support advancing medical technology in multiple ways. Firstly, machine vision algorithms assist ophthalmologists to detect vascular retinopathy in eye fundus photographs. Similar algorithms can also help with histological cell type recognition in microscopy images. Furtermore, image segmentation algorithms can be used in medical images for organ segmentation, or even tumor segmentation. This helps radiologists tremendously when interpreting these images.
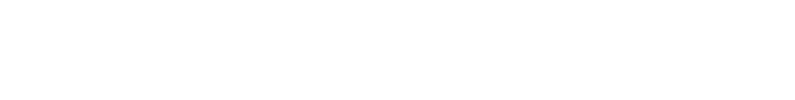
In addition, advanced search and optimization algorithms can support doctors to optimize medicine dosages or even treatment strategies for individual patients. Finally, pattern recognition algorithms can also allow to extract valuable information from proxy measurements. The following figure illustrates this idea.
The following example illustrates how pattern recognition algorithms can allow to extract valuable information form proxy measurements.
Blood pressure measurements deliver important information. Unfortunately, one of the shortcomings of traditional blood pressure measurements is that it only allows measuring a snapshot of the patient’s condition. They do not allow to track minute to minute blood pressure evolution over an extended period of time. This problem is being solved by using PPG (photoplethysmographic) signals as a proxy for blood pressure. With each cardiac cycle the heart pumps blood distending the arteries and arterioles in the subcutaneous tissue. The change in volume caused by the pressure pulse is detected by illuminating the skin with a light-emitting diode (LED) and then measuring the amount of back scattered light with a photodiode. This system is already implemented in numerous health-tracking and sports watches. Although these applications mainly focus on extracting the heart rate from the PPG signal, extracting more valuable information from PPG data is an active area of research.
Numerous companies and institutions (including Verhaert) are advancing medical technology by extracting additional information such as blood pressure from these signals. Even, detecting heart diseases based on PPG data becomes quite possible. The benefits are clear: PPG measurements are cheap and convenient for patients and medical professionals and the continuous tracking provides a deeper insight into the patient’s condition (read more about this project).
Artificial intelligence is proving to be a powerful tool in solving the medical challenges of the future: delivering higher quality care to an aging population with less medical professionals, while keeping the cost manageable. All stakeholders will benefit. First of all, the patient’s quality of life will be improved and prolonged with high quality, personalized care and early illness detection. On the other hand, medical professionals will have access to high quality tools and technological support. Moreover, governments and health insurances can optimize efficiency in patient care and treatment. This might become crucial in keeping social security sustainable.
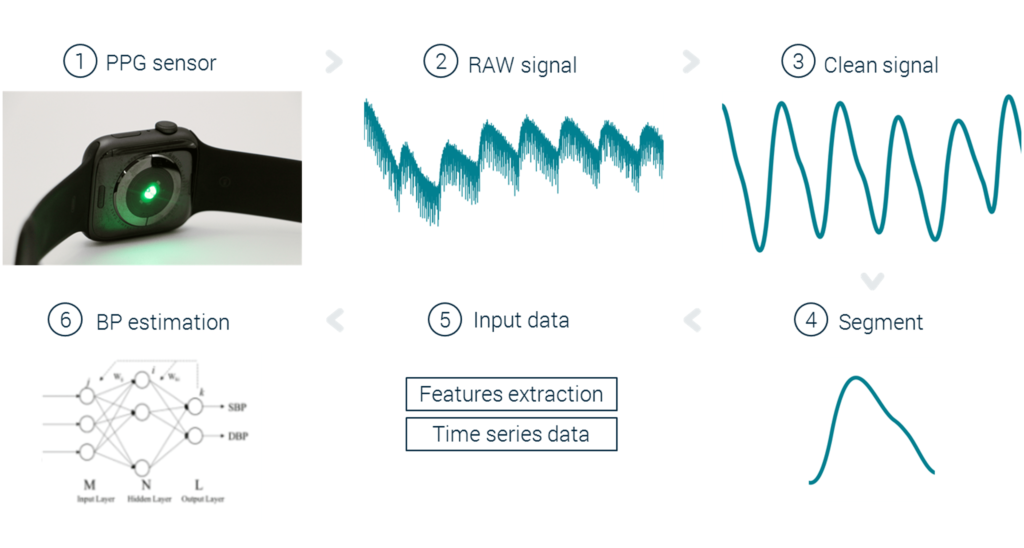
The challenge of AI
Advancing medical technology by incorporating Artificial Intelligence in its applications comes with challenges. Developing such applications demands a multidisciplinary approach. Knowledge of data gathering, often sensor design and signal processing, needs to be combined with setting up an IT infrastructure for data transaction, data storage, aggregation and processing this data. Merely focusing on the technical side of the problem will not deliver a profitable, successful solution. You need a profound understanding of your new business case, the user and the use case and, of course, the technical challenge.
A deep understanding of the users and the role of AI in the use case is necessary to deliver value. Application development will
require collaboration of nurses, doctors and medical institutions for gathering data, use case investigation, medical expertise and AI-prototype testing to answer the following questions.
-
- Which information does the user need and in what format?
- When does the user need this information?
- What does the user aim to do with this information?
- Is the user ready to implement the use of this information?
- How do we assure the collaboration of nurses, doctors and hospitals in the product development?
- Can you assure collaboration of nurses, doctors and hospitals in the data gathering phase
A data driven medical application has to comply with both the Medical Device Directive (93/42/EEC, depending on the medical claims made) and the regulations regarding protection of personal data (General Data Protection Regulation, GDPR). A quality management system conform ISO 13485 will be required, and setting up and maintaining these systems requires expertise and investments.
The approach
Coping with the complexity of developing a medical device, specifically one that incorporates AI systems, demands a structured project approach, as you want to avoid endless trial & error iterations. The project team needs to develop all process steps congruently to develop insights in the complete process, from data collection to the implementation of the result in the practical workflow of the medical professional.
In practice, this requires an iterative design approach, a design space exploration exercise and a proof of concept phase to fail fast and cheap. You have to identify issues before they become too difficult and costly to resolve.
The iterative design phase
Start with analysing the business case and the users problem. Based on this analysis, the first solution concepts are generated. Evaluating these options requires relevant data. Within clinical trials, this is a difficult and expensive process, which is why it is often not opportune to fully dive into this task so soon in the project. There are readily available data sources such as MIMIC I-II-III, Kaggle and DERMnet, among others that eachcontain valuable data for different medical fields such as dermatology, cardiology, pulmonology, oncology, spinal surgery, …
These online data platforms allow building fast proof of concepts of a first AI-model to start learning. These first explorative steps are crucial to gain insight in all steps of the entire process before starting detailed development of individual aspects. Furthermore, it enables evaluating the product early on with all stakeholders and provides a first opportunity to identify possible problems for workflow integration, ergonomics or sources of data bias. It is crucial to check for blind spots in the data. For example, which patient profiles are underrepresented in the data? Are there relevant patient variables omitted from the data set? Machine learning applications cannot learn outside of the data provided, so it is crucial to ensure high data quality for the algorithm to be successful.
The information gained in these first steps is crucial in setting up the data gathering campaign. In this step, high quality, reliable data has to be collected, as it will form the basis of the algorithm development. It requires collaboration of medical professionals and material and procedures suitable for the data collection in their workflow. Other than that, this step requires guarantees that the patient information will be treated according to the data protection regulations. To obtain the collaboration of both medical professionals and patients, it is necessary to visualize their benefits in previous iterations. At the same time, these steps allow the technical team to gain deeper insight in the problem and to mitigate technical risks.
Design Space exploration
What do you do when you start developing and you realize close to your deadline that your system didn’t meet the requirements? What to do when you discover at the end of the project that the user’s problem is not properly solved?
Just like the development of other technical systems, the time and effort invested in designing and training an AI system is considerable. As a result, selecting the wrong or suboptimal combination of subsystems can cost a lot of time and money.
Early design space exploration can reduce this risk by first mapping all functions that your system requires (ie dividing your application in subsystems), which helps to start ideating & scouting alternatives. The objective of this step is to assure alignment of all application components.
There are myriad of possible AI algorithms. Choosing the right algorithm for your application demands a profound understanding of the technical problem and the user’s needs.
Typical questions in the first phase of problem understanding and data understanding involve:
-
- Classification or regression problem
- Model evaluation approach (metric)
- Understanding of available features
- Volume of the available data and the difficulty of obtaining more data (or augmenting the available data)
Once you have chosen the algorithm approach, there are still have many more choices to make. Let’s say you have chosen to implement an artificial neural network over alternatives, such as a support vector machine, regression trees, … You now need to establish an architecture and a hyperparameter set.
The optimal architecture and hyperparameter set cannot be ‘calculated’ on beforehand. Tuning these parameters is a work relying on insight of the AI engineer and a rigorous and structured optimization approach. Choices need to made and tested regarding the activation function (ReLU, tanh), architecture (number of hidden layers, fully connected layers, convolutional layers,…), optimization algorithms and anti-overfitting techniques (drop-out, regularization, …). The number of possible combinations is virtually endless.
Choosing between these parameters is a difficult trade-off between model performance, avoiding over-fitting of the data, memory and computational restrictions, time delay acceptable for evaluating the model, among others.
A structured design space exploration method ensures that you explore the different possibilities without sticking to the most familiar (or trendy) solution. Due to personal bias, people often think that what they know is better than the unknown. Therefore, a structured design exploration is highly recommended.
Conclusion
Medical innovation has accomplished remarkable feats in the past decades. Historical progress has always been based on evidence provided by data. Nowadays, AI advances enable opportunities to speed up this progress and to open new possibilities. Artificial Intelligence will start advancing medical technology, creating preventive and personalized medicine. To make full use of these opportunities, companies need to embrace a structured multidisciplinary innovation approach, combining expertise in fields ranging from AI, sensors, data engineering, electronics over human factor engineering and medical science up to legal regulations.
Download the perspective